Vascular surgery is a specialized field of medicine that focuses on the treatment of diseases affecting the circulatory system, including arteries, veins, and lymphatic vessels. This branch of surgery addresses a wide range of conditions, from life-threatening aneurysms to common varicose veins. Understanding the role of vascular surgery, the various procedures involved, and what to expect during recovery can help patients make informed decisions about their treatment.
What is Vascular Surgery?
Vascular surgery involves the diagnosis and surgical management of diseases affecting the vascular system, which includes the arteries, veins, and lymphatic vessels. Unlike other systems of the body, which may rely on the assistance of other organs (such as the lungs or heart), the vascular system is an independent network that facilitates the circulation of blood and lymph. Any blockage, narrowing, or dysfunction in the vascular system can result in severe complications, ranging from pain to life-threatening emergencies like strokes or heart attacks.
A vascular surgeon is trained to perform surgeries that restore and maintain proper blood flow throughout the body. This may involve bypassing blocked arteries, repairing damaged blood vessels, or removing problematic veins. Importantly, vascular surgeons can treat both acute and chronic conditions using a variety of techniques, from traditional open surgery to minimally invasive procedures.
Why is Vascular Surgery Important?
The health of the vascular system is crucial for overall well-being. Blood vessels are responsible for transporting oxygen and nutrients to organs and tissues, as well as removing waste products. When the vascular system is compromised, the consequences can be far-reaching. For example, restricted blood flow to the limbs can result in pain, tissue damage, or even amputation. Problems in the carotid arteries (the arteries in the neck that supply blood to the brain) can lead to strokes, while issues in the abdominal aorta (the large artery that supplies blood to the lower body) can cause life-threatening aneurysms.
Vascular diseases can be caused by a variety of factors, including genetic predisposition, lifestyle choices, and other health conditions such as diabetes, high blood pressure, or smoking. Age is also a significant factor, with vascular problems becoming more common as people get older.
For individuals suffering from vascular disease, surgery can be a critical intervention to prevent complications, improve quality of life, and even save lives. Vascular surgeons are equipped to offer both preventive care, such as screenings and lifestyle recommendations, as well as advanced surgical interventions.
Common Vascular Conditions Treated by Surgery
- Aneurysms: An aneurysm occurs when a blood vessel wall weakens, causing it to balloon outward. This can happen in any artery, but it is most commonly seen in the aorta. If an aneurysm ruptures, it can lead to life-threatening internal bleeding. Vascular surgeons can repair aneurysms using techniques such as endovascular aneurysm repair (EVAR) or open surgery.
- Peripheral Artery Disease (PAD): PAD occurs when the arteries that supply blood to the legs and feet become narrowed or blocked due to atherosclerosis (a buildup of plaque). Symptoms include leg pain, cramping, and ulcers. Surgical treatments for PAD include angioplasty, stenting, and bypass surgery.
- Carotid Artery Disease: The carotid arteries supply blood to the brain. If these arteries become narrowed due to plaque buildup, it can lead to a stroke. Carotid endarterectomy and carotid artery stenting are two common surgical procedures used to treat this condition.
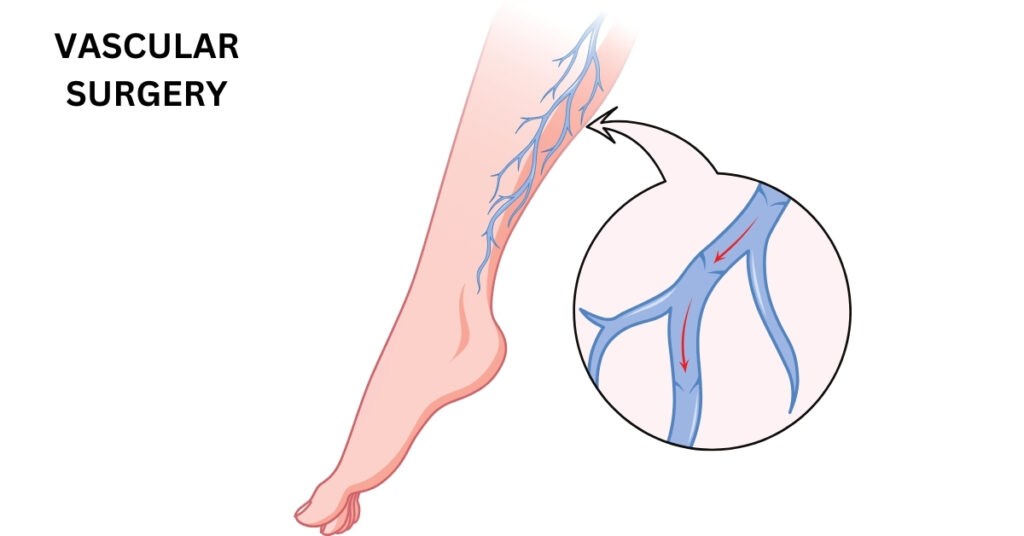
- Varicose Veins: Varicose veins are swollen, twisted veins that usually occur in the legs. While often seen as a cosmetic issue, they can cause pain, swelling, and other complications. Treatments include sclerotherapy, laser therapy, and vein stripping.
- Deep Vein Thrombosis (DVT): DVT occurs when a blood clot forms in a deep vein, typically in the legs. If the clot breaks free, it can travel to the lungs and cause a pulmonary embolism, a potentially fatal condition. Treatment may involve anticoagulants or, in severe cases, surgery to remove the clot.
- Chronic Venous Insufficiency (CVI): CVI occurs when the veins in the legs fail to efficiently return blood to the heart, leading to swelling, pain, and ulcers. Treatments include compression therapy and surgery to improve vein function.
- Lymphedema: Lymphedema is a condition where excess lymphatic fluid accumulates in tissues, causing swelling, often in the arms or legs. Vascular surgeons can perform procedures to help improve lymphatic drainage.
Types of Vascular Surgery Procedures
Vascular surgeons have several options when it comes to treating vascular conditions. The choice of procedure depends on the condition, its severity, and the patient’s overall health. Some of the most common vascular surgery procedures include:
- Angioplasty and Stenting: This minimally invasive procedure involves using a balloon to open up a narrowed artery. A stent (a small mesh tube) is often inserted to keep the artery open.
- Endovascular Aneurysm Repair (EVAR): EVAR is a minimally invasive technique used to treat aneurysms in the aorta. It involves inserting a graft (a fabric tube) into the aneurysm through a small incision in the groin, which reinforces the weakened artery wall.
- Bypass Surgery: In cases where an artery is completely blocked, bypass surgery may be performed. This involves creating a detour around the blocked artery using a graft, either from the patient’s own veins or a synthetic material.
- Carotid Endarterectomy: This procedure involves removing plaque from the carotid artery to prevent strokes.
- Sclerotherapy: Sclerotherapy is used to treat varicose veins and spider veins. A solution is injected into the vein, causing it to collapse and fade from view.
- Vein Stripping and Ligation: This procedure is used to remove or tie off large varicose veins.
- Thrombectomy: Thrombectomy involves surgically removing a blood clot from a blood vessel.
Recovery After Vascular Surgery
Recovery after vascular surgery varies depending on the type of procedure performed and the patient’s overall health. Minimally invasive procedures, such as angioplasty, typically have shorter recovery times compared to open surgeries. Patients may be able to return to normal activities within a few days or weeks. However, more complex surgeries, like bypass or aneurysm repair, may require longer recovery times, sometimes up to several months.
Key Tips for Post-Surgery Recovery
- Follow your surgeon’s instructions: After surgery, it’s important to follow all instructions regarding medication, wound care, and activity restrictions.
- Stay active, but rest when needed: Light physical activity, such as walking, can help improve circulation and prevent complications like blood clots. However, avoid strenuous activities until cleared by your surgeon.
- Eat a healthy diet: A diet rich in fruits, vegetables, lean proteins, and whole grains can promote healing and reduce the risk of further vascular problems.
- Monitor for complications: Watch for signs of infection, such as redness, swelling, or fever, and seek medical attention if you notice anything unusual.
- Attend follow-up appointments: Regular checkups with your vascular surgeon are crucial to ensure the success of the procedure and monitor for any potential issues.
Conclusion
Vascular surgery plays a vital role in maintaining the health of the circulatory system. Whether it’s treating life-threatening conditions like aneurysms or addressing less serious but painful issues like varicose veins, vascular surgery provides patients with a range of options for improving their quality of life. If you or a loved one is dealing with a vascular condition, consulting with a qualified vascular surgeon is the first step toward better health and recovery.